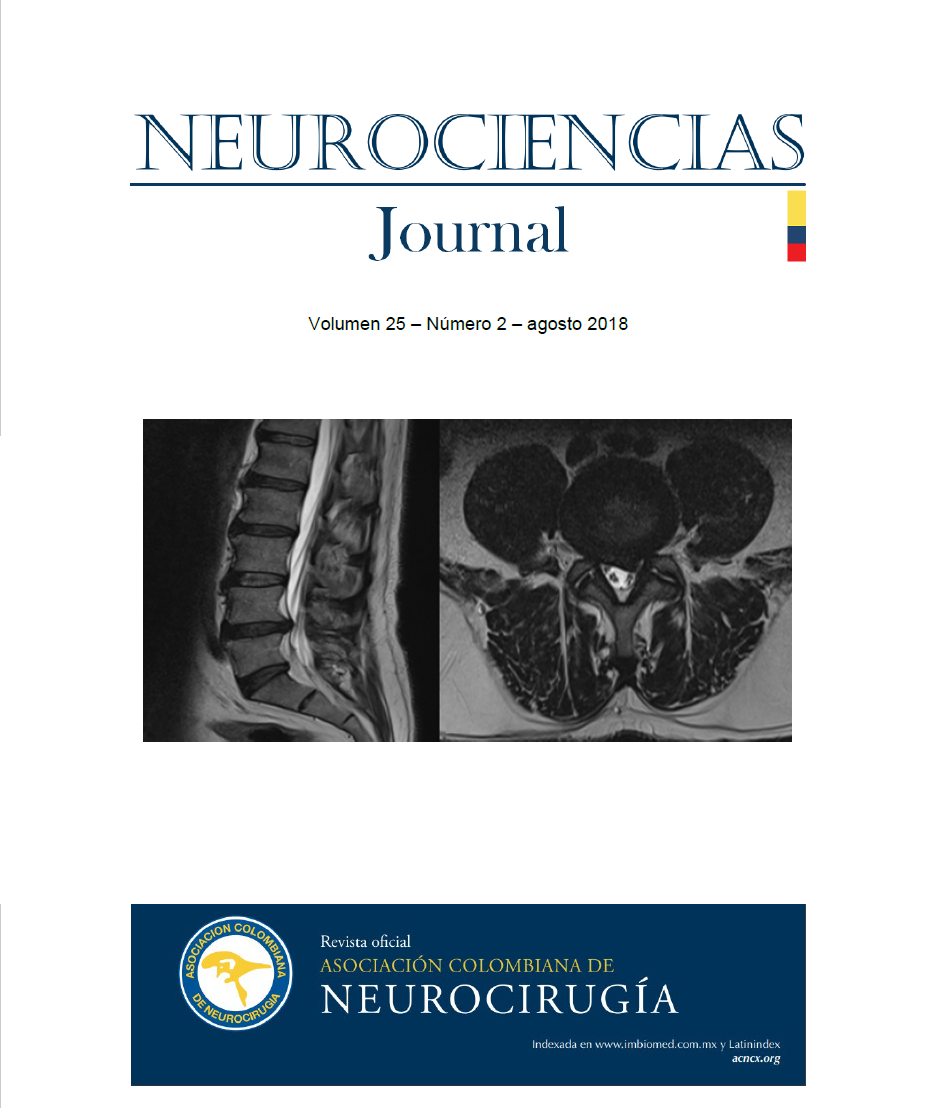
NEUROCISTICERCOSIS SUBARACNOIDEA ASOCIADA A COLECCIÓN SUBDURAL: REPORTE DE CASO
DOI:
https://doi.org/10.51437/nj.v25i2.52Palabras clave:
neurocisticercosis, colección subdural, escólex, epilepsiaResumen
La neurocisticercosis subaracnoidea es una causa frecuente de epilepsia que rara vez se asocia con colecciones subdurales. Se presenta el caso de un paciente con neurocisticercosis asociada a colección subdural a quien se le realizo craniectomía, fenestración y capsulectomía con buen desenlace.
Citas
World Health Organization (2016): Taeniasis/cysticercosis [En línea] WHO. https://www.who.int/es/news-room/fact-sheets/detail/taeniasis-cysticercosis [Accedido 20 octubre. 2019].
Fernández R, González-Fernández C (2017). Neurocisticercosis: una enfermedad que no debemos olvidar. Galicia Clin 2017; 78 (3):116-122.
Kimura-Hayama, E, Higuera, J (2010). Neurocysticercosis: Radiologic-Pathologic Correlation RadioGraphics Vol. 30 No. 6 https://doi.org/10.1148/rg.306105522
Flores. M (2013). Cisticercosis humana en Venezuela un problema de salud olvidado. [En línea]. http://maiquiflores.over-blog.es/article-cisticercosis-humana-en-venezuela-un-problema-de-salud-olvidado-119788739.html. [Accedido 20 octubre. 2019].
Mahale Rohan, Mehta Anish (2015). Extraparenchymal (Racemose) Neurocysticercosis and Its Multitude Manifestations: A Comprehensive Review J Clin Neuro . doi: 10.3988/jcn.2015.11.3.203
Debacq. Gabrielle, Moyano. Luz M. (2017). Systematic review and meta-analysis estimating association of cysticercosis and neurocysticercosis with epilepsy NEGLECTED TROPICAL DISEASES https://dx.doi.org/10.1371%2Fjournal.pntd.0005153.
Carabin H1, Ndimubanzi PC, (2011). Clinical manifestations associated with neurocysticercosis: a systematic review. Neglected tropical diseases https://doi.org/10.1371/journal.pntd.0001152
Jing-Long Zhao, Alexander Lerner (2015). Review Imaging spectrum of neurocysticercosis radiology of infectious diseases. elservier https://doi.org/10.1016/j.jrid.2014.12.001
A. Clinton White, Jr. Christina M. Coyle (2018). Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). doi:10.4269/ajtmh.18-88751
So-hyang IM, Seong-ho Park, (2005) Subdural cysticercosis mimicking a chronic subdural hematoma J Neurosurg 102:389, 2005 https://doi.org/10.3171/jns.2005.102.2.0389
Nash Theodore, Garcia Hector (2011). Diagnosis and Treatment of Neurocysticercosis Nat Rev Neurol doi: 10.1038/nrneurol.2011.135
Rajshekhar V. (2001) Cerebral cysticercus granuloma associated with a subdural effusion. Neurol India 2001;49:182 http://www.neurologyindia.com/text.asp?2001/49/2/182/1268
Pamplona Jaime , Braz Ana (2015). A rare case of racemose neurocysticercosis and its complications. Case report Neuroradiol J doi: 10.1177/1971400915595305
Fernández R, González-Fernández C (2017). Neurocisticercosis: una enfermedad que no debemos olvidar. Galicia Clin 2017; 78 (3):116-122.
Kimura-Hayama, E, Higuera, J (2010). Neurocysticercosis: Radiologic-Pathologic Correlation RadioGraphics Vol. 30 No. 6 https://doi.org/10.1148/rg.306105522
Flores. M (2013). Cisticercosis humana en Venezuela un problema de salud olvidado. [En línea]. http://maiquiflores.over-blog.es/article-cisticercosis-humana-en-venezuela-un-problema-de-salud-olvidado-119788739.html. [Accedido 20 octubre. 2019].
Mahale Rohan, Mehta Anish (2015). Extraparenchymal (Racemose) Neurocysticercosis and Its Multitude Manifestations: A Comprehensive Review J Clin Neuro . doi: 10.3988/jcn.2015.11.3.203
Debacq. Gabrielle, Moyano. Luz M. (2017). Systematic review and meta-analysis estimating association of cysticercosis and neurocysticercosis with epilepsy NEGLECTED TROPICAL DISEASES https://dx.doi.org/10.1371%2Fjournal.pntd.0005153.
Carabin H1, Ndimubanzi PC, (2011). Clinical manifestations associated with neurocysticercosis: a systematic review. Neglected tropical diseases https://doi.org/10.1371/journal.pntd.0001152
Jing-Long Zhao, Alexander Lerner (2015). Review Imaging spectrum of neurocysticercosis radiology of infectious diseases. elservier https://doi.org/10.1016/j.jrid.2014.12.001
A. Clinton White, Jr. Christina M. Coyle (2018). Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). doi:10.4269/ajtmh.18-88751
So-hyang IM, Seong-ho Park, (2005) Subdural cysticercosis mimicking a chronic subdural hematoma J Neurosurg 102:389, 2005 https://doi.org/10.3171/jns.2005.102.2.0389
Nash Theodore, Garcia Hector (2011). Diagnosis and Treatment of Neurocysticercosis Nat Rev Neurol doi: 10.1038/nrneurol.2011.135
Rajshekhar V. (2001) Cerebral cysticercus granuloma associated with a subdural effusion. Neurol India 2001;49:182 http://www.neurologyindia.com/text.asp?2001/49/2/182/1268
Pamplona Jaime , Braz Ana (2015). A rare case of racemose neurocysticercosis and its complications. Case report Neuroradiol J doi: 10.1177/1971400915595305
Descargas
Publicado
2019-12-05
Cómo citar
Ferrer, X. (2019). NEUROCISTICERCOSIS SUBARACNOIDEA ASOCIADA A COLECCIÓN SUBDURAL: REPORTE DE CASO. Neurociencias Journal, 25(2), 73–79. https://doi.org/10.51437/nj.v25i2.52
Número
Sección
Artículo de casos y series de casos