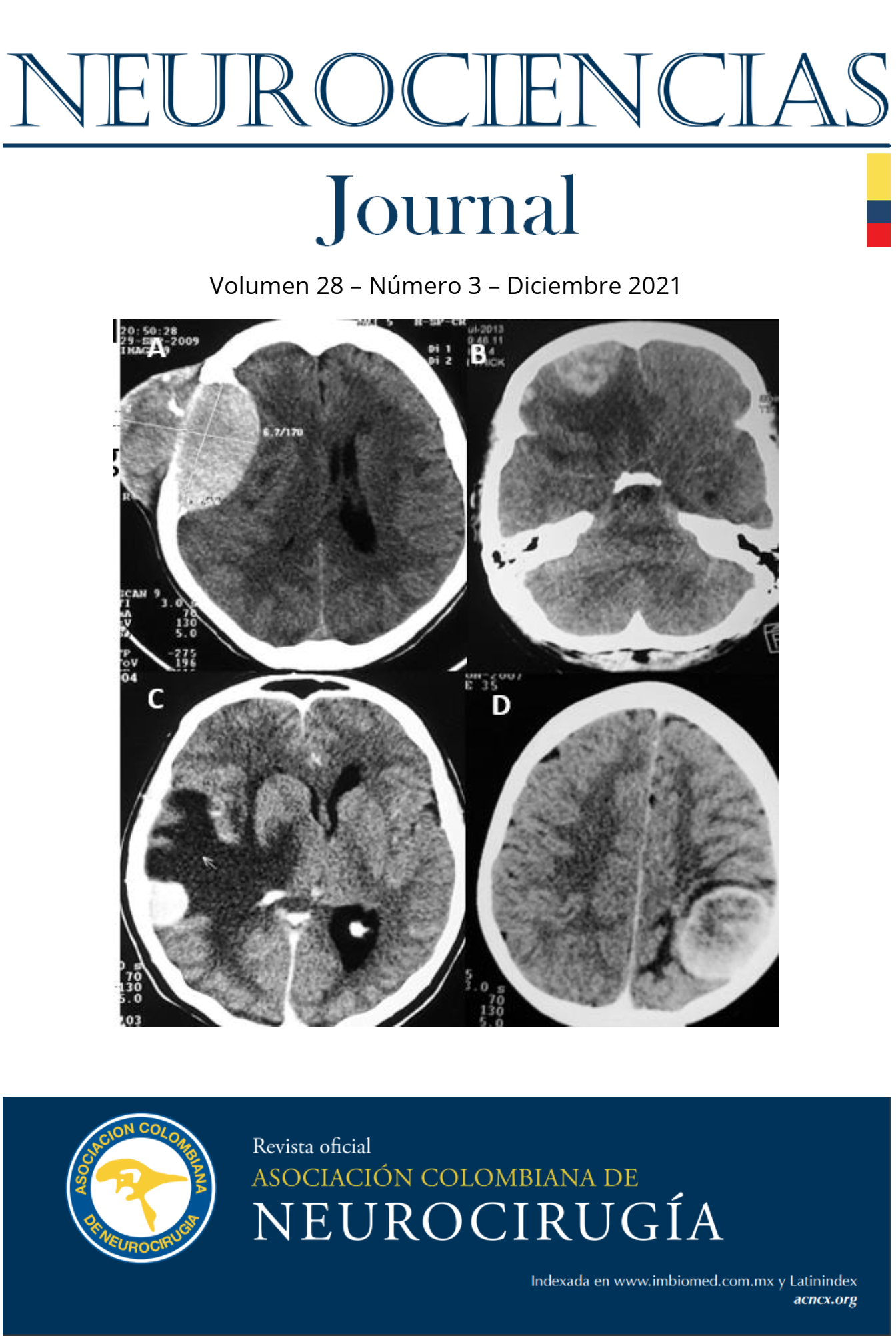
LESIÓN TUMEFACTA DESMIELINIZANTE: REVISIÓN BIBLIOGRÁFICA
DOI:
https://doi.org/10.51437/nj.v28i3.182Palabras clave:
Glioma, Esclerosis Múltiple, Linfoma, DesmielinizanteResumen
Resumen
La lesión tumefacta desmielinizante es una variedad rara de la esclerosis múltiple, cuya fisiopatología no ha sido dilucidada. Son lesiones poco frecuentes, con una prevalencia cercana a los 0.3 casos por 100.000 habitantes. Su clínica corresponde a la de una lesión espacio ocupante cerebral de aspecto tumoral, y a pesar de considerarse una variante de la Esclerosis Múltiple (EM), no traduce la sintomatología típica de la misma. Por las razones anteriores, constituye un reto diagnóstico y terapéutico dada su similitud con patologías neoplásicas de sistema nervioso central, especialmente el glioma. Con el presente trabajo se pretende hacer una revisión de esta patología y ofrecer una herramienta para el diagnóstico, haciendo hincapié en las herramientas imagenológicas a fin de favorecer el tratamiento y minimizar en lo posible procedimientos invasivos.
Abstract
The Tumefactive Demyelinating Lesion (TDL) is a rare variety of Multiple Sclerosis (MS), whose physiopathology has not been yet dilucidated. Its prevalence is close to 0.3 per 100.000 habitants. Its clinical presentation is that of a space occupying lesion, and despite being a variety of MS, it doesn´t manifest the typical symptomatology. Given these reasons, it constitutes a diagnostic and therapeutic challenge, since it easily resembles central nervous system neoplastic pathologies, for example, gliomas. In this paper we aim to deliver a diagnostic and therapeutic tool, highlighting the process based in imagenologic devices to avoid unnecessary invasive procedures.
Resumo
A lesão inchada desmielinizante e uma variante esquisita da Esclerose Múltipla, cuja fisiopatologia não foi elucidada ainda. A sua prevalência está perto de 0.3/100.000 habitantes. Sua manifestação clínica e duma lesão espaço ocupante, e ainda sendo variante da MS, não presenta seus sintomas clássicos. E por isto, que o diagnóstico e o tratamento e um reto, especialmente porque simula patologias neoplásicas do Sistema nervosa central como o glioma. Neste artigo, tentamos fazer uma ferramenta diagnostica e terapêutica, sublinhando a utilização de técnicas de imagens para evitar os procedimentos invasivos.
Citas
Abdoli, M., Freedman, M.S., 2015. Neuro-oncology dilemma: Tumour or
tumefactive demyelinating lesion. Mult Scler Relat Disord 4, 555–566.
https://doi.org/10.1016/j.msard.2015.07.013
Algahtani, H., Shirah, B., Alassiri, A., 2017. Tumefactive demyelinating lesions: A
comprehensive review. Mult Scler Relat Disord 14, 72–79.
https://doi.org/10.1016/j.msard.2017.04.003
Barbosa, B.C., Marchiori, E., Leal Leidersnaider, C., Brandao, L., Castillo, M., 2019.
Demyelinating lesions behaving like aggressive tumours on advanced MRI
techniques. Neuroradiol J 32, 103–107.
https://doi.org/10.1177/1971400919826394
Butteriss, D.J.A., Ismail, A., Ellison, D.W., Birchall, D., 2003. Use of serial proton
magnetic resonance spectroscopy to differentiate low grade glioma from
tumefactive plaque in a patient with multiple sclerosis. Br J Radiol 76, 662–
https://doi.org/10.1259/bjr/85069069
Chiavazza, C., Pellerino, A., Ferrio, F., Cistaro, A., Soffietti, R., Rudà, R., 2018.
Primary CNS Lymphomas: Challenges in Diagnosis and Monitoring.
Biomed Res Int 2018, 3606970. https://doi.org/10.1155/2018/3606970
Dobson, R., Giovannoni, G., 2019. Multiple sclerosis - a review. Eur J Neurol 26,
–40. https://doi.org/10.1111/ene.13819
Fan, X., Mahta, A., De Jager, P.L., Kesari, S., 2012. Rituximab for tumefactive
inflammatory demyelination: a case report. Clin Neurol Neurosurg 114,
–1328. https://doi.org/10.1016/j.clineuro.2012.03.010
Frederick, M.C., Cameron, M.H., 2016. Tumefactive Demyelinating Lesions in
Multiple Sclerosis and Associated Disorders. Curr Neurol Neurosci Rep 16,
https://doi.org/10.1007/s11910-016-0626-9
Hardy, T.A., Chataway, J., 2013. Tumefactive demyelination: an approach to
diagnosis and management. J Neurol Neurosurg Psychiatry 84, 1047–
https://doi.org/10.1136/jnnp-2012-304498
Ikeguchi, R., Shimizu, Y., Abe, Kayoko, Shimizu, S., Maruyama, T., Nitta, M., Abe,
Koichiro, Kawamata, T., Kitagawa, K., 2018. Proton magnetic resonance
spectroscopy differentiates tumefactive demyelinating lesions fromNeurociencias Journal Vol 28Núm 3 Esquivel M y Arriola J.
Página | 111
gliomas. Mult Scler Relat Disord 26, 77–84.
https://doi.org/10.1016/j.msard.2018.08.025
Jain, R.S., Khan, I., Kandelwal, K., Desai, T., 2017. Tumefactive demyelinating
lesions (TDLs): A case series of clinicoradiological features. Clin Neurol
Neurosurg 162, 91–94. https://doi.org/10.1016/j.clineuro.2017.09.013
Kepes, J.J., 1993. Large focal tumor-like demyelinating lesions of the brain:
intermediate entity between multiple sclerosis and acute disseminated
encephalomyelitis? A study of 31 patients. Ann Neurol 33, 18–27.
https://doi.org/10.1002/ana.410330105
Kim, D.S., Na, D.G., Kim, K.H., Kim, J.-H., Kim, E., Yun, B.L., Chang, K.-H., 2009.
Distinguishing tumefactive demyelinating lesions from glioma or central
nervous system lymphoma: added value of unenhanced CT compared
with conventional contrast-enhanced MR imaging. Radiology 251, 467–
https://doi.org/10.1148/radiol.2512072071
La Mantia, L., Tramacere, I., Firwana, B., Pacchetti, I., Palumbo, R., Filippini, G.,
Fingolimod for relapsing-remitting multiple sclerosis. Cochrane
Database Syst Rev 4, CD009371.
https://doi.org/10.1002/14651858.CD009371.pub2
Mujic, A., Liddell, J., Hunn, A., McArdle, J., Beasley, A., 2002. Non-neoplastic
demyelinating process mimicking a disseminated malignant brain
tumour. J Clin Neurosci 9, 313–317.
https://doi.org/10.1054/jocn.2001.0961
Nayak, L., Reardon, D.A., 2017. High-grade Gliomas. CONTINUUM: Lifelong
Learning in Neurology 23, 1548.
https://doi.org/10.1212/CON.0000000000000554
Neuroimmunology Group of Neurology Branch of Chinese Medical Association,
Neuroimmunology Committee of Chinese Society for Immunology,
Immunology Society of Chinese Stroke Association, 2017. Chinese
Guidelines for the Diagnosis and Management of Tumefactive
Demyelinating Lesions of Central Nervous System. Chin Med J (Engl) 130,
–1850. https://doi.org/10.4103/0366-6999.211547
Pakos, E.E., Tsekeris, P.G., Chatzidimou, K., Goussia, A.C., Markoula, S.,
Argyropoulou, M.I., Pitouli, E.G., Konitsiotis, S., 2005. Astrocytoma-like
multiple sclerosis. Clin Neurol Neurosurg 107, 152–157.
https://doi.org/10.1016/j.clineuro.2004.06.003
POPE, W.B., BRANDAL, G., 2018. Conventional and advanced magnetic
resonance imaging in patients with high-grade glioma. Q J Nucl Med Mol
Imaging 62, 239–253. https://doi.org/10.23736/S1824-4785.18.03086-8Neurociencias Journal Vol 28Núm 3 Esquivel M y Arriola J.
Página | 112
QI, W., JIA, G., WANG, X., ZHANG, M., MA, Z., 2015. Cerebral tumefactive
demyelinating lesions. Oncol Lett 10, 1763–1768.
https://doi.org/10.3892/ol.2015.3481
Sánchez, P., Meca-Lallana, V., Barbosa, A., Manzanares, R., Palmí, I., Vivancos, J.,
Tumefactive demyelinating lesions of 15 patients: Clinicoradiological features, management and review of the literature. J Neurol
Sci 381, 32–38. https://doi.org/10.1016/j.jns.2017.08.005
Seifert, C.L., Wegner, C., Sprenger, T., Weber, M.S., Brück, W., Hemmer, B.,
Sellner, J., 2012. Favourable response to plasma exchange in tumefactive
CNS demyelination with delayed B-cell response. Mult Scler 18, 1045–
https://doi.org/10.1177/1352458511429012
Suh, C.H., Kim, H.S., Jung, S.C., Choi, C.G., Kim, S.J., 2018. MRI Findings in
Tumefactive Demyelinating Lesions: A Systematic Review and MetaAnalysis. AJNR Am J Neuroradiol 39, 1643–1649.