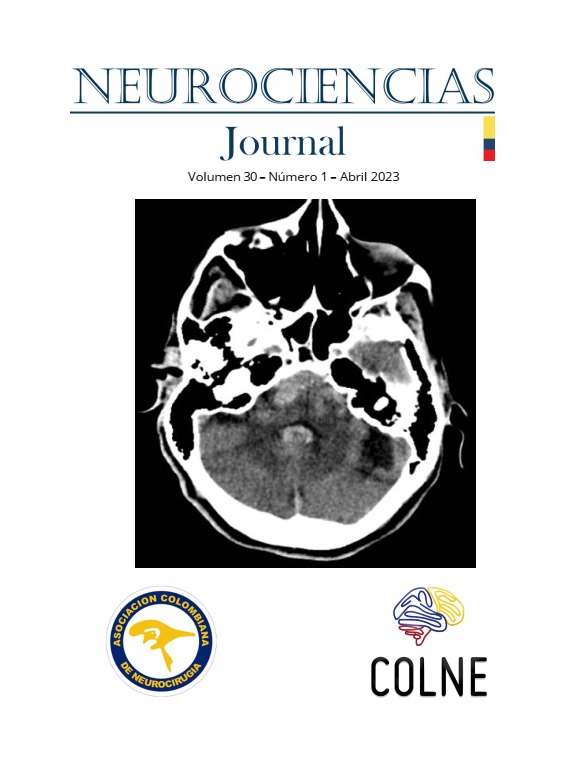
REPORTE DE CASO DE: EVOLUCION ATIPICA DE ENCEFALITIS DE RASMUSSEN.
DOI:
https://doi.org/10.51437/nj.v30i1.422Palabras clave:
Estatus epileptico, Encefalitis de Rasmussen, Epilepsia parcial continuaResumen
Resumen (Español)
Introducción: La encefalitis de Rasmussen es una entidad severa y poco frecuente, que predomina en la infancia. Su etiología es desconocida. Se caracteriza por ser una enfermedad progresiva, y por afectar un hemisferio, en forma de epilepsia parcial continua farmacorresistente, y atrofia hemisférica unilateral. A largo plazo deja secuelas neurológicas, lo que conlleva a una discapacidad desde una edad temprana.
Materiales y Métodos: Es un artículo de caso, sobre la evolución de un paciente con Encefalitis de Rasmussen.
Resultados: Se reporta un paciente de 9 años con una evolución atípica de la enfermedad, quien ha estado libre de crisis en más de 2 años y en monoterapia con bajas dosis de medicación.
Conclusiones: El reconocimiento y manejo temprano de esta patología incide en pronostico y complicaciones de un paciente con encefalitis de Rasmussen.
Palabras clave: Estatus epilepticus; Encefalitis de Rasmussen; Epilepsia parcial continua
Abstract (English)
Introduction: Rasmussen encephalitis is a severe and rare entity that predominates in childhood. Its etiology is unknown. It is characterized by being a progressive disease, and by affecting one hemisphere, in the form of drug-resistant continuous partial epilepsy, and unilateral hemispheric atrophy. In the long term, it leaves neurological consequences, which leads to disability from an early age.
Materials and Methods: It is a case report, on the evolution of a patient with Rasmussen Encephalitis.
Results: A 9-year-old patient is reported with an atypical evolution of the disease, who has been seizure-free for more than 2 years and on monotherapy with low doses of medication.
Conclusions: Early recognition and management of this pathology affects the prognosis and complications of a patient with Rasmussen encephalitis.
Keywords: Status epilepticus; Rasmussen encephalitis; Epilepsy partialis continua
Resumo (Português)
Introdução: A encefalite de Rasmussen é uma entidade grave e rara que predomina na infância. Sua etiologia é desconhecida. Caracteriza-se por ser uma doença progressiva e por afetar um hemisfério, na forma de epilepsia parcial contínua resistente a medicamentos e atrofia hemisférica unilateral. A longo prazo deixa sequelas neurológicas, que levam à incapacidade desde cedo.
Materiais e Métodos: É um artigo de caso, sobre a evolução de um paciente com Encefalite de Rasmussen.
Resultados: É relatado um paciente de 9 anos com evolução atípica da doença, há mais de 2 anos sem crises e em monoterapia com baixas doses de medicação.
Conclusões: O reconhecimento e tratamento precoce desta patologia afeta o prognóstico e as complicações de um paciente com encefalite de Rasmussen.
Palavras-chave: Estado de mal epiléptico; encefalite de Rasmussen; Epilepsia parcial contínua
Citas
Zuberi SM, Wirrell E, Yozawitz E, et al. ILAE classification and definition of epilepsy syndromes with onset in neonates and infants: Position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63(6):1349-1397. doi:10.1111/epi.17239
Bien CG, Tiemeier H, Sassen R, et al. Rasmussen encephalitis: Incidence and course under randomized therapy with tacrolimus or intravenous immunoglobulins. Epilepsia. 2013;54(3):543-550. doi:https://doi.org/10.1111/epi.12042
Varadkar S, Bien CG, Kruse CA, et al. Rasmussen’s encephalitis: clinical features, pathobiology, and treatment advances. Lancet Neurol. 2014;13(2):195-205. doi:10.1016/S1474-4422(13)70260-6
Tang C, Luan G, Li T. Rasmussen’s encephalitis: mechanisms update and potential therapy target. Ther Adv Chronic Dis. 2020;11:2040622320971413. doi:10.1177/2040622320971413
Ai J, Wang Y, Liu D, et al. Genetic Factors in Rasmussen’s Encephalitis Characterized by Whole-Exome Sequencing. Front Neurosci. 2021;15:744429. doi:10.3389/fnins.2021.744429
Westfall JJ, Schwind WN, Sran S, et al. Molecular and spatial heterogeneity of microglia in Rasmussen encephalitis. Acta Neuropathol Commun. 2022;10(1):168. doi:10.1186/s40478-022-01472-y
Orsini A, Foiadelli T, Carli N, et al. Rasmussen’s encephalitis: From immune pathogenesis towards targeted-therapy. Seizure. 2020;81:76-83. doi:https://doi.org/10.1016/j.seizure.2020.07.023
Bien CG, Widman G, Urbach H, et al. The natural history of Rasmussen’s encephalitis. Brain. 2002;125(8):1751-1759. doi:10.1093/brain/awf176
Holec M, Nagahama Y, Kovach C, Joshi C. Rethinking the MRI findings in early Rasmussen encephalitis: a case report and review of the current literature. Pediatr Neurol. 2016;59:85-89. doi:https://doi.org/10.1016/j.pediatrneurol.2015.12.004
Wang ZI, Krishnan B, Shattuck DW, et al. Automated MRI Volumetric Analysis in Patients with Rasmussen Syndrome. AJNR Am J Neuroradiol. 2016;37(12):2348-2355. doi:10.3174/ajnr.A4914
Cay-Martinez KC, Hickman RA, II GMM, Provenzano FA, Sands TT. Rasmussen Encephalitis: An Update. 2020;40:201-210. doi:https://doi.org/ 10.1055/s-0040-1708504. ISSN 0271-8235.
Lagarde S, Boucraut J, Bartolomei F. Medical treatment of Rasmussen’s Encephalitis: A systematic review. Rev Neurol (Paris). 2022;178(7):675-691. doi:https://doi.org/10.1016/j.neurol.2022.01.007
Bellamkonda N, Phillips HW, Chen JS, et al. Epilepsy surgery for Rasmussen encephalitis: the UCLA experience. J Neurosurg Pediatr PED. 2020;26(4):389-397. doi:https://doi.org/10.3171/2020.4.PEDS2098
Bien CG, Granata T, Antozzi C, et al. Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: a European consensus statement. Brain J Neurol. 2005;128(Pt 3):454-471. doi:10.1093/brain/awh415
Dalby T, Wohl E, Dinsmore M, Unger Z, Venkatraghavan T. Pathophysiology of Cerebral Edema—A Comprehensive Review. J Neuroanaesth Crit Care. 2020;8:163-172. doi:https://doi.org/ 10.1055/s-0040-1721165
Sanoussi S, Comet C, Kaefer K, Attou R, De Bels D, Gazagnes MD, Honoré PM RS. Can Magnetic Resonance Imaging make the Differential Diagnosis between Cerebral Ischemia and Epilepsy? J Transl Int Med. 2019;7(4):123-125. doi:10.2478/jtim-2019-0025
Fernández IS, Goodkinc HP, Scott RC. Pathophysiology of convulsive status epilepticus. Seizure Eur J Epilepsy. 2019;6:16-21. doi:https://doi.org/10.1016/j.seizure.2018.08.002
Maramattom BV, Rao T. Cortical unihemispheric brain edema (CUBE) due to a multi-system inflammatory syndrome in adults (MIS-A). Epileptic Disord. 2022;24(3):595-601. doi:10.1684/epd.2022.1429
Bhargava H, Dwivedi D. Hemiconvulsion-hemiplegia-epilepsy Syndrome: A Case Series. J Pediatr Neurosci. 2020;15(3):274-278. doi:10.4103/jpn.JPN_27_19
Sánchez-Espino LF, Ivars M, Antoñanzas J BE. Sturge-Weber Syndrome: A Review of Pathophysiology, Genetics, Clinical Features, and Current Management Approache. Appl Clin Genet. 2023;16:63-81. doi:https://doi.org/10.2147/TACG.S363685
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Neurociencias Journal

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.